
Walking into a store, eatery or nightspot around Butte County, a casual observer might assume the pandemic has passed. Quite the contrary: Absences of face coverings and plexiglass barriers belie a new spike in COVID-19 cases that has renewed worries among local health officials.
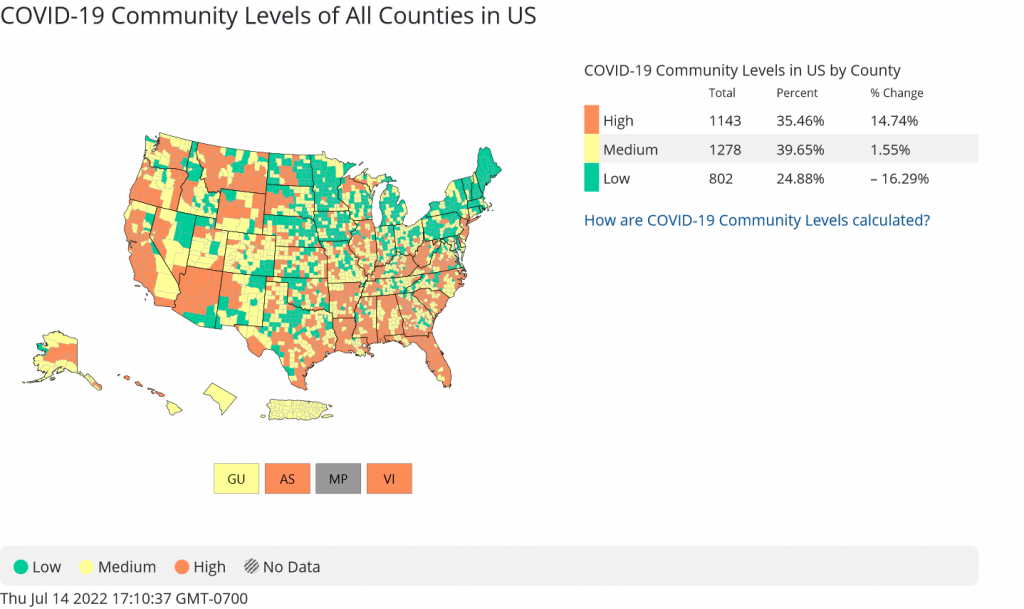
As of July 14, Butte County re-entered the U.S. Centers for Disease Control and Prevention’s “high” classification for COVID-19 Community Level.
For a three-month span through July 13 (the most recent date reported on the county’s COVID dashboard), Butte County Public Health (BCPH) recorded 4,873 new cases—roughly 10 percent of the amount since the start of the pandemic in March 2020. That total, 45,569, includes probable cases as well as confirmed. This figure is probably low, according to BCPH, missing patients who test positive at home, do not seek treatment and don’t report results.
The original virus has mutated into various strains; the one spreading widely across the U.S., omicron, has several subvariants that have proven highly transmissible and resistant to immunity. Vaccinated, boosted and even previously ill patients are coming down with COVID this summer when exposed to omicron BA.4 and BA.5, the latter dominating cases across the country.
These substrains combined with our “new normal” to yield a fresh spike.
“I’m concerned,” said Dr. Linda Lewis, epidemiologist with BCPH.
As is Dr. Marcia Nelson, chief medical officer at Enloe Medical Center and a physician in general practice. Patients admitted into Chico’s hospital for COVID care has jumped in the past month, from around 10 a day to between 15 and 19.
“It’s still a very significant illness,” she said. “It’s still having very significant impacts. It still can cause long COVID, it still can send people into the hospital and it still can kill people.”
Hospitalizations have jumped countywide, from single digits a day in May to 30 last week. Omicron is less lethal but still taking lives—10 since April 10. Since the beginning of the outbreak, COVID has caused or contributed to the deaths of 558 county residents.
BCPH is tracking three substrains: BA.2, BA.4 and BA.5. For patients and physicians, the distinction matters little.
“It doesn’t really make a difference in clinical advice or how we’re doing clinical investigations,” Lewis explained. “COVID is COVID. But we [in public health] like to keep track of which variants are circulating because it gives us a view of what to expect.”
Take BA.5—as those cases rise, Lewis continued, health officials anticipate more reinfections since that substrain has demonstrated “the ability to evade immune response” developed through vaccination or contracting the virus previously. (Nelson referred to this phenomenon as “immune escape.”) The most recent genetic sequencing results, from June, indicate BA.5 is causing around 22 percent of COVID cases in the county, compared to nearly 70 percent for BA.2, which first appeared in March.
Underreporting of cases—potentially by a factor of 10, Lewis said—complicates tracking the current surge, BCPH projects subsidence locally in early August. However, returns to school and college later in the month may push another upswing.
“Fortunately there’s something different this time around,” Nelson said. “Our experience [at the hospital] with prior COVID waves is that the patients were very, very sick; they oftentimes required intensive care unit management. Fortunately it’s the vast minority of patients who require this level of care [now] … the current variants and subvariants are causing less severe illness than the variants we were dealing with in the winter time a year ago.
“So that’s good for everyone.”
Prevention matters
At her family medicine practice, where she sees patients in the afternoon, Nelson is seeing “many, many more patients who are calling in having tested positive for COVID.” She discusses whether they should seek treatments such as Paxlovid, an oral antiviral medication, and monoclonal antibodies (MAB), an injection or infusion, to reduce the duration and impact of infection.
“The illness is less severe, but the illness is still very significant,” she said—knowledge also born of personal experience. Nelson caught COVID, and as she recovered, she missed more work than from any other illness.
As such, she joined Lewis in reemphasizing the preventative measures health officials promoted at the height of the pandemic: namely, vaccines and face coverings.
Both doctors encouraged people who to get fully vaccinated and boosted according to their eligibility. Thought they still offer protection against the variant, vaccines out now have not been formulated for omicron; manufacturers Moderna and Pfizer are in the process of testing new versions, targeting release by winter. BCPH closed its Chico vaccine clinic June 30 citing the availability of vaccines countywide.
The CDC recommends second boosters for adults 50 and older along with “some people” 12 and older “who are moderately or severely immunocompromised.”
In Butte County, 41 percent of residents remain unvaccinated. Just over half (54 percent) are fully vaccinated, and just over half of those (58 percent) received booster doses. The statewide vaccination rate is 71 percent—Butte ranks 46th out of 58 counties.
“Taking advantage of the excellent science that has come about, and taking advantage of these vaccines that reduce the severity of illness and the deaths from COVID, that’s the low-hanging fruit here,” Nelson said. “If we could all just agree that we’re going to listen to the science, listen to the research, get vaccinated, protect ourselves and each other, that would go far.”
Lewis agreed, adding: “I think we are more vulnerable in Butte County than in other areas of the state where vaccination rates are higher. So I remain concerned. It will impact—and we’re seeing it now—our long-term care and skilled nursing facilities as they deal with waves of BA.5 coming through. And even if it doesn’t hospitalize [someone], it can be really disruptive to someone’s life.”
She notices “very few people” wearing masks indoors, despite recommendations from public health, as well as resumptions of public gatherings—“I think that very much is related to the increase in cases.” To build immunity across the community, Lewis referred to the “Swiss cheese model”: layering multiple slices to cover the holes in one.
“We have vaccines, we have masking, we have distancing, we have improved ventilation,” she continued. “All of those can decrease the spread and are really important in decreasing that spread.”



Be the first to comment