
For Mike Wiltermood, the COVID-19 spike that’s gripping Butte County and the rest of the world is more than just a professional concern. It’s personal.
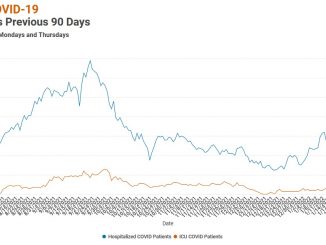
Wiltermood knows the numbers. He’s seen people they represent firsthand. As President/CEO of Enloe Medical Center, he’s watched them fill the emergency room and the intensive care unit of his hospital, pushing the number of coronavirus patients beyond the high marks set last winter, when state officials placed the North State in the tightest tier of pandemic restrictions.
Things have gotten so bad that Enloe announced Monday (Sept. 13) that, due to national shortages, it anticipates rationing a treatment that reduces COVID’s severity to the extent of precluding hospitalizations.
Also on Monday, Butte County Public Health (BCPH) announced that the surge has reaped a steep increase in fatalities. There have been 23 COVID deaths since Aug. 1—two more than the previous five months combined—bringing the county’s total to 225. BCPH said in a news release it expects the trend to continue due to the high number of hospitalizations since August.
Wiltermood also knows well the emotional toll of coronavirus—the experience of losing someone. Last year, before vaccinations became available, a close friend from high school contracted COVID. He was “a very healthy individual,” said Wiltermood, who was acquainted with his whole family.
“He was texting a lot of us as he was going through this, and so we got sometimes hour-by-hour reports. It was scary and it was lonely [for him] to die the way he did.
“It’s not a good death,” Wiltermood added. “The oxygen depletion does a number on you.”
Enloe and especially BCPH have encouraged the public to get vaccinated. Indeed, now with the highly transmissible delta variant of the virus entrenched in Butte County, they’re all but pleading, with Dr. Linda Lewis saying in Monday’s news release on fatalities, “Tragically, many of these deaths could have been avoided if more people had been vaccinated.” Of the 25 county residents under 80 who’ve died from COVID since April 15, only one was fully vaccinated.
Though half of his relatives are “against government overreach, [have] conservative politics … felt like they didn’t trust some of the institutions we should be trusting, the CDC and the FDA,” Wiltermood said, all went for vaccinations after his friend’s death.
“I hope it doesn’t take an up-close-and-personal experience like that for people to get vaccinated.”
Disproportionate drag
As of Tuesday afternoon, Butte County had 17,685 cases reported since the start of the pandemic with 879 people in isolation and 106 in county hospitals. The final week in August brought 949 new cases, second only to the 966 recorded the week before Christmas. Last week (Sept. 7-13), the county had 647; during that time, Enloe reported caring for 72 hospitalized patients a day—12 a day in critical care, five on ventilators.
Dr. Marcia Nelson, chief medical officer at Enloe, spoke in a recent interview with the CN&R about the effectiveness of monoclonal antibody (MAB) infusions in reducing the severity of sickness of COVID-positive people, whether vaccinated or unvaccinated, which in turn has kept patients out of hospital wards.

However, Enloe’s Monday announcement indicated “rationing of this treatment is imminent” because the U.S. Department of Health and Human Services told the medical center it may not receive its full allocation. As such, MAB “can no longer be relied upon as your first defense against serious illness, hospitalization or long-term health consequences. It is imperative that you vaccinate as soon as possible.”
The rub is that Butte County lags much of California in vaccination rates. Latest numbers from BCPH show 52.85 percent of eligible residents—i.e., ages 12 and up—fully vaccinated and 7.61 percent partially vaccinated. Statewide, those figures are 68.5 percent and 9.9 percent, respectively, putting the county more than 15 points off the pace and in the bottom third of counties. That lack of protection, combined with the arrival of the delta variant of COVID—which currently accounts for a projected 98 percent of the cases here—has left Butte County especially vulnerable.
“The only way out of this is for people to get vaccinated,” Nelson said. “By people’s choices to get vaccinated, they’re standing with me, they’re standing with us in the health-care community, trying to take care of all these patients.”
Nelson shared the same message with a patient in her family medicine practice. She reviewed medical research on the vaccines, then shared how much the pandemic weighs on her and her colleagues “living COVID 24 hours a day, seven days a week”:
Statistics fluctuate daily, but consistently, around 90 percent of Enloe’s coronavirus patients are unvaccinated, including virtually all in the ICU. Today (Sept. 15), that figure is 81 percent unvaccinated or not fully vaccinated of the 74 hospitalized.) They’re “sicker,” Nelson said, and constitute “the vast majority of patients who are here in the hospital.”
Moreover, with schools back in session, “I fully expect we’re going to have even more of a surge,” she added, “because these are the age of kids who can’t be vaccinated … and they’ll take it back to their parents, 50 percent of whom are unvaccinated.”
Balancing act
Even within health care, support for vaccination isn’t universal. Last month, a large group of North State nurses gathered outside Enloe to protest California’s vaccine mandate for medical workers. That requirement takes effect Sept. 30. More than 100 opponents of the vaccine requirement, including registered nurses from Enloe and Oroville Hospital, picketed in August.
According to Enloe, 95 percent of its active physicians and 76 percent of employees are fully vaccinated, with another 2 percent of employees partially vaccinated. The prospect of losing vaccine-hesitant caregivers, in an area already challenged for recruitment, looms surprisingly low among the hospital’s concerns.

“It’s daunting to think how many [more] COVID patients we could have,” Wiltermood said. “What that means for us: It doesn’t matter if we felt fully staffed or not … we have to start rationing services—we have to start cutting back on elective cases, for sure—and we have plans in place for all that, for redeploying resources as more and more COVID cases come in.
“I think that’s the major issue, not whether someone decides to work here because they need to be vaccinated or not. I think the big picture is, scores of people coming into the hospital when we’re already stretched to our capacity.”
Wiltermood added that “just a handful of employees have been very, very adamant about not getting vaccinated and worried about the state mandate.” Nelson said administrators try to address these reservations by sharing “the science”; but, ultimately, there’s only so much the hospital can do.
“Nobody is going to sit down and force somebody, against their will, to get a shot put in their arm. People get to choose,” she continued. “It’s a privilege to work in health care, and with that privilege comes the responsibility to get vaccinated against COVID.”
Danette York, county public health director, said her department along with local hospitals would continue to promote vaccinations—to staff and to the public. That was even before she revealed at a Sept. 1 news conference that she’d contracted COVID-19. Being fully vaccinated, she told local media her symptoms have been milder than those generally experienced by unvaccinated patients.
In her interview with the CN&R, York said the mandate “does put us in a difficult position” because public health departments approach outbreaks broadly “to protect the public. Not very often are we treating an individual person,” she continued, but that’s what the state requirement entails with health-care providers.
“From a local public health leader position—and this is getting into my own personal opinion—I like to provide options whenever possible,” York said. “I am not on a fly on the wall; I don’t know what has happened or what discussions have happened or what researches have happened at the state level for them to make this decision. I can only hope they have looked at every alternative possible to determine if there was a way to provide options for people.”
That said, York affirmed her support for vaccination. Looking at percent vaccinated amid the surge, she said, “it’s not enough; we want more. That’s why we have so much focus on taking the vaccine to different groups and meeting them where they’re at” with mobile clinics along with community clinics and pharmacies.
Nelson, Enloe’s chief medical officer, is blunt in her assessment of current critical situation: “When people don’t get vaccinated, or people who don’t get vaccinated don’t wear their masks, that’s really breaking the back of our health-care system. Because that’s really so fragile right now.”



Be the first to comment